HardKnocks
Forum Lieutenant
- 121
- 33
- 28
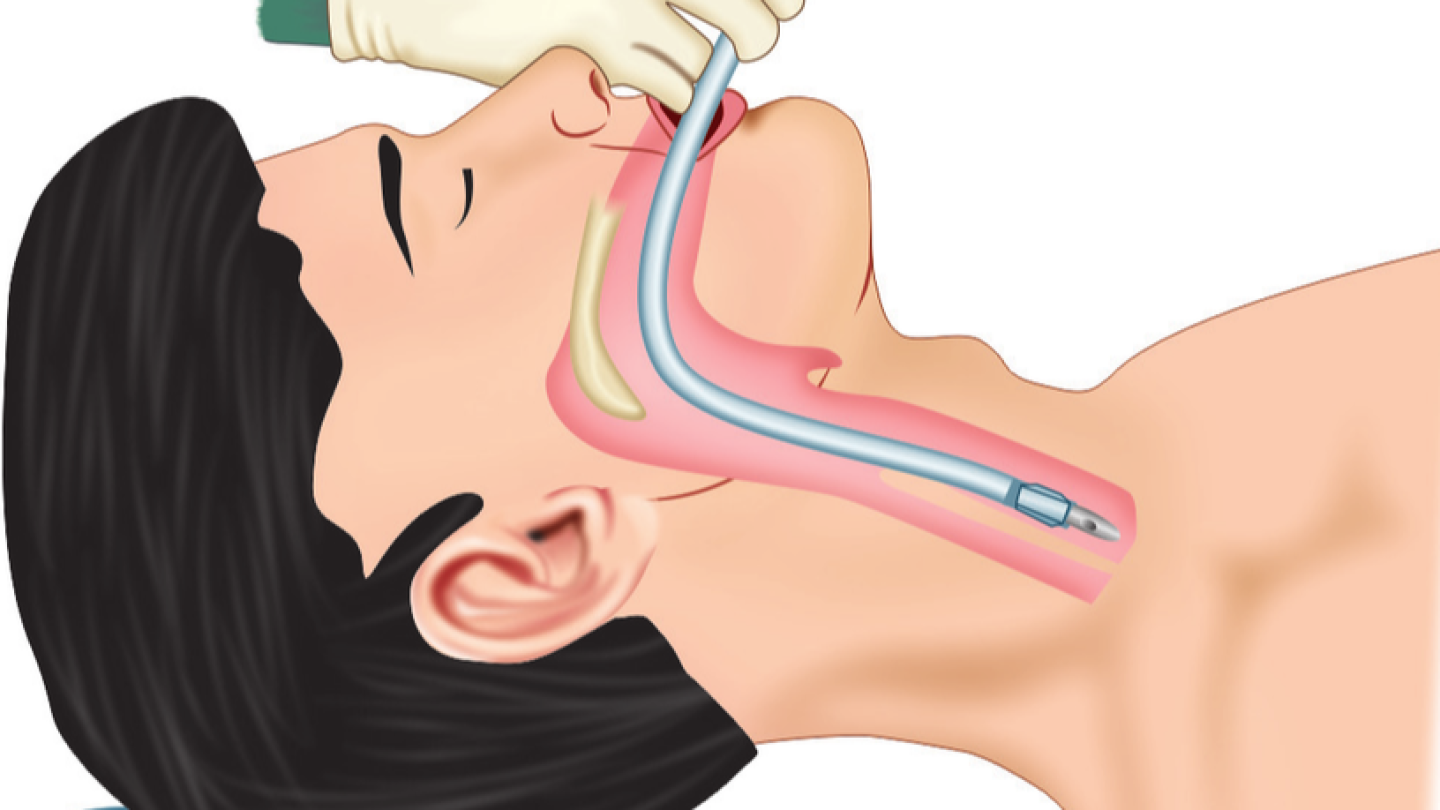
I have seen EMT's successfully use Supraglottic Airways, (i.e. I-Gel) and its been an approved Skill in various States.
Personally I love the I-Gel. Its almost fool-proof compared to Intubation with a Blade-King Airway, (i.e. no over depth insertion issues and no Right Bronchi Entries etc). As we all know Intubation is a very perishable skill.
I don't agree with the discussion; "BVM is Not Taught Well" included in the Aug 2021 National EMS Scope of Practice Model 2019: Including Change Notices 1.0 and 2.
How do they qualify that statement? BVM use is a mandatory Pass/Fail EMT Skill.
If certain local training is not adequate or substandard, conduct a review/audit and fix it. Don't make blanket statements that are all encompassing.
How many of you practice in a State that approves and uses them for EMT and/or Paramedics';
If not; Do you support expanding EMT's Scope of Practice to include Supraglottic Airways for EMTs.
As an EMT I've been brought up amd worked most of the time alongside the .Mil Crowd. I've seen 19-25 year old do some incredible saves during Field Trauma work.
Why is there a spectrum of our EMS Community that is so hesitant in advancing new skill sets? Remember when TCCC was first introduced?
Thoughts/Ideas?
HK
Personally I love the I-Gel. Its almost fool-proof compared to Intubation with a Blade-King Airway, (i.e. no over depth insertion issues and no Right Bronchi Entries etc). As we all know Intubation is a very perishable skill.
I don't agree with the discussion; "BVM is Not Taught Well" included in the Aug 2021 National EMS Scope of Practice Model 2019: Including Change Notices 1.0 and 2.
How do they qualify that statement? BVM use is a mandatory Pass/Fail EMT Skill.
If certain local training is not adequate or substandard, conduct a review/audit and fix it. Don't make blanket statements that are all encompassing.
The use of supraglottic airways (SGA) and waveform capnography at the EMT level was extensively debated. Several public commenters expressed lack of support on draft language that proposed to add them to the interpretive guidelines for EMTs during the national engagement period. The expert panel was evenly divided on the topic. Several “pros” and “cons” for adding SGA and waveform capnography for EMTs at the national level were considered. It was noted that several jurisdictions are already using SGA as a more definitive airway than the BVM although some panelists added that the BVM is not taught well or used effectively in many cases. Major “cons” point to a critical patient safety concern if an SGA is not placed properly or is not verified using waveform capnography. Many felt the education for SGA and waveform capnography would add significant time and increase expense to the EMT program, a consideration that was worrisome and expressed by the public and members of the expert panel. Others suggested that BVM ventilation may not be done well, but a misplaced advanced airway could lead to no ventilation and patient detriment or demise. Finally, a limited review of the literature highlights the fact there is a general lack of evidence that SGA improves outcomes in cardiac arrest or other etiologies over BVM ventilation. The expert panel concluded that while SGA and waveform capnography could successfully be taught and measured at the EMT level, it is an intervention that should be reserved for an experienced practitioner and therefore, is not a prudent addition as an entry-level skill to the Practice Model for an EMT now. Some States currently allow licensed EMTs to use SGA and/or waveform capnography although this activity is dependent on strict oversight by a physician medical director and is not permitted in all jurisdictions.
How many of you practice in a State that approves and uses them for EMT and/or Paramedics';
If not; Do you support expanding EMT's Scope of Practice to include Supraglottic Airways for EMTs.
As an EMT I've been brought up amd worked most of the time alongside the .Mil Crowd. I've seen 19-25 year old do some incredible saves during Field Trauma work.
Why is there a spectrum of our EMS Community that is so hesitant in advancing new skill sets? Remember when TCCC was first introduced?
Thoughts/Ideas?
HK