zzyzx
Forum Captain
- 428
- 90
- 28
You are an NP or a PA working on an ambulance. Imagine that it is a trial program like the one in Orange County, CA.
How would you handle the following 911 calls:
1) Which would you treat and not transport (with referral to PMD)?
2) Which would need an ER eval?
3) Which would be a likely hospital admission?
1) 35 y/o diabetic (Type I) with a fingerstick glucose of 400; ran out of his insulin. Asymptomatic.
2) 55 y/o c/o hypertension, BP 245/120, asymptomatic. Was a relative's house and tried their automatic BP. Does not take any anti-hypertensives and has not seen a doctor in years.
2) Patient involved in a fight. C/o a "fight bite." He punched someone in the mouth and has lacerations on his hand. "Do I need to see my doc to get antibiotics or will I be okay without?"
3) Diabetic (Type II) who takes metformin, glypizide, and an insulin was found ALOC by his wife. Blood glucose 20. After you administer dextrose, he is fully alert and oriented.
4) Twenty year old with a sore throat x 3 days. Also fever. No SOB and vital signs stable. Says she can't deal with the pain anymore; no OTC meds working.
5) 7 y/o SOB with Hx asthma. Pt is acting age appropriate and does not appear to be in acute distress. Mild retractions noted and tachypnea; bilateral exp wheeze. SpO2 95% after breathing Tx.
6) CHF'er who has frequently visited the ER and is well known to the staff. C/o just not feeling well, generalized weakness, increased dyspnea on exertion. Vital signs stable; no acute distress. Denies chest pain. 12-lead shows paced rhythm.
7) Pt was running on the beach when she stepped on and broke a bottle. Has deep lac on foot requiring suturing. Bleeding controlled.
8) 27 y/o syncopal episode at work. Vital signs stable; asymptomatic. No prior Hx.
9) 35 y/o c/o fever, malaise, cough x 3 days. The cough is productive with green phlegm. SpO2 99% and stable vital signs. C/o mild SOB but is in no acute distress.
10) New first-time parents of a 20 day old with fever 102. Vital signs are stable and the baby does not appear to be in any distress.
11) Auto mechanic c/o injection-gun injury to his hand. Pt was using a high-pressure grease gun when it injected grease into his hand. Minimal pain. No loss of function. Pt states he called because his co-worker told him that the grease could enter his blood stream and cause a stroke.
12) 3 y/o with fever x 2 days. Mother states that she has given him Tylenol several times but his fever keeps coming back. No coughing, no retractions, no signs of respiratory distress. Child is smiling at you and interacting normally with mother. All vital signs are WNL except that temperature is 102 and pt is a little tachycardic.
13) 28 y/o male with chest pain and SOB. Pain increases with deep inhalation. 12 lead unremarkable. Pt is mildly tachycardic and tachypneic but not in any acute distress. Lung sounds clear to auscultation. SpO2 99%.
14) 15 y/o with testicle pain x 1 hour. No penile discharge or dysuria.
15) 2 y/o fell off high chair onto hard kitchen floor. Pt has hematoma to occipital region of his head. Pt is acting age appropriate and was crying immediately after the fall. No vomiting. Mother asks, "Does he need a cat scan? Can we let him sleep?"
How would you handle the following 911 calls:
1) Which would you treat and not transport (with referral to PMD)?
2) Which would need an ER eval?
3) Which would be a likely hospital admission?
1) 35 y/o diabetic (Type I) with a fingerstick glucose of 400; ran out of his insulin. Asymptomatic.
2) 55 y/o c/o hypertension, BP 245/120, asymptomatic. Was a relative's house and tried their automatic BP. Does not take any anti-hypertensives and has not seen a doctor in years.
2) Patient involved in a fight. C/o a "fight bite." He punched someone in the mouth and has lacerations on his hand. "Do I need to see my doc to get antibiotics or will I be okay without?"
3) Diabetic (Type II) who takes metformin, glypizide, and an insulin was found ALOC by his wife. Blood glucose 20. After you administer dextrose, he is fully alert and oriented.
4) Twenty year old with a sore throat x 3 days. Also fever. No SOB and vital signs stable. Says she can't deal with the pain anymore; no OTC meds working.
5) 7 y/o SOB with Hx asthma. Pt is acting age appropriate and does not appear to be in acute distress. Mild retractions noted and tachypnea; bilateral exp wheeze. SpO2 95% after breathing Tx.
6) CHF'er who has frequently visited the ER and is well known to the staff. C/o just not feeling well, generalized weakness, increased dyspnea on exertion. Vital signs stable; no acute distress. Denies chest pain. 12-lead shows paced rhythm.
7) Pt was running on the beach when she stepped on and broke a bottle. Has deep lac on foot requiring suturing. Bleeding controlled.
8) 27 y/o syncopal episode at work. Vital signs stable; asymptomatic. No prior Hx.
9) 35 y/o c/o fever, malaise, cough x 3 days. The cough is productive with green phlegm. SpO2 99% and stable vital signs. C/o mild SOB but is in no acute distress.
10) New first-time parents of a 20 day old with fever 102. Vital signs are stable and the baby does not appear to be in any distress.
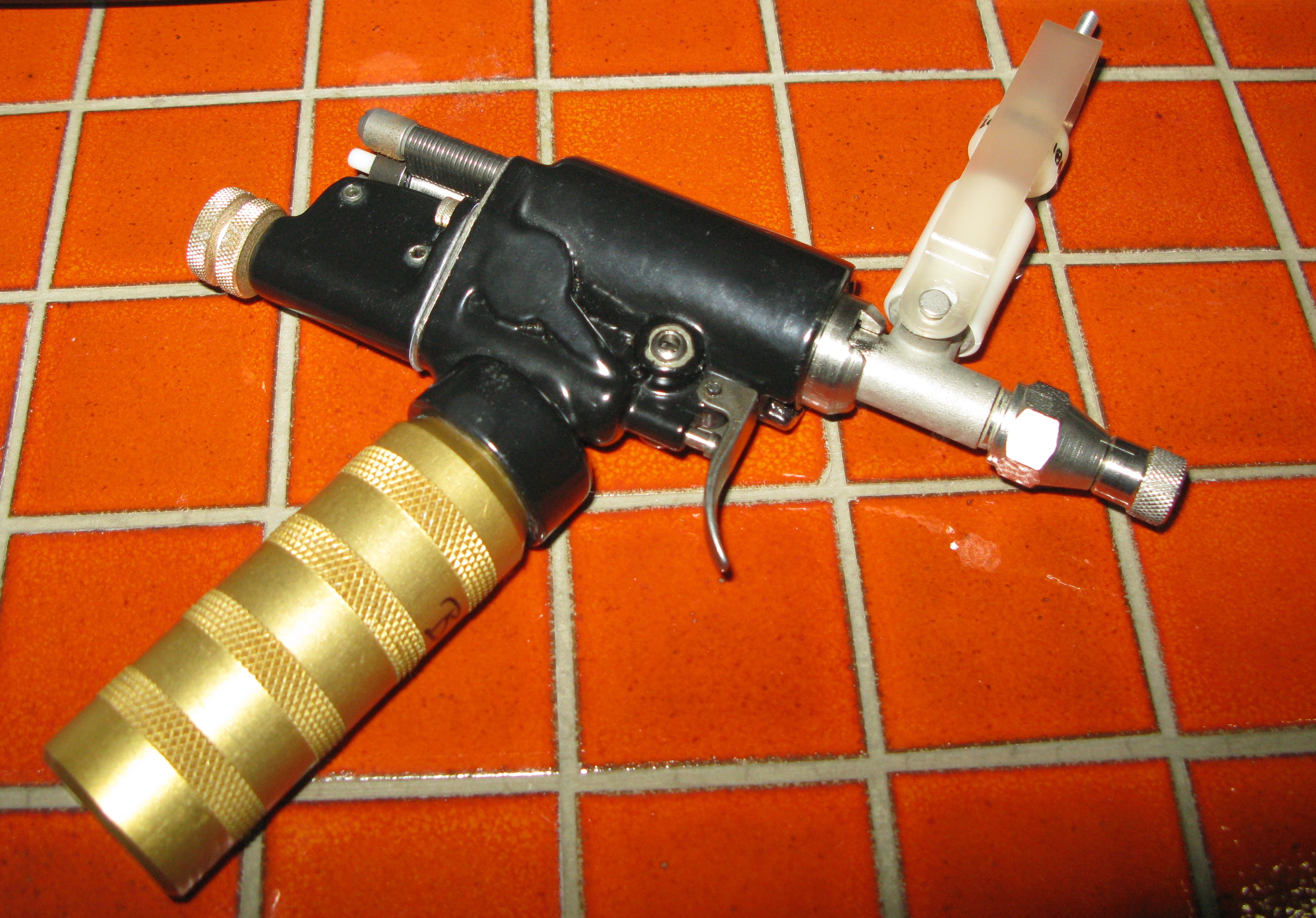
11) Auto mechanic c/o injection-gun injury to his hand. Pt was using a high-pressure grease gun when it injected grease into his hand. Minimal pain. No loss of function. Pt states he called because his co-worker told him that the grease could enter his blood stream and cause a stroke.
12) 3 y/o with fever x 2 days. Mother states that she has given him Tylenol several times but his fever keeps coming back. No coughing, no retractions, no signs of respiratory distress. Child is smiling at you and interacting normally with mother. All vital signs are WNL except that temperature is 102 and pt is a little tachycardic.
13) 28 y/o male with chest pain and SOB. Pain increases with deep inhalation. 12 lead unremarkable. Pt is mildly tachycardic and tachypneic but not in any acute distress. Lung sounds clear to auscultation. SpO2 99%.
14) 15 y/o with testicle pain x 1 hour. No penile discharge or dysuria.
15) 2 y/o fell off high chair onto hard kitchen floor. Pt has hematoma to occipital region of his head. Pt is acting age appropriate and was crying immediately after the fall. No vomiting. Mother asks, "Does he need a cat scan? Can we let him sleep?"