tpchristifulli
Forum Crew Member
- 36
- 16
- 8
Dispatched to an assisted living center for a 70 yr female pt with shortness of breath, diarrhea, and vomiting.Pt has normal mental status.
Upon arrival you find your patient sitting in her recliner in obvious distress. She states she feels very nauseated and sick to her stomach. Onset of this morning upon waking up. Hx of LBBB and implanted pace maker.
You palpate a pulse of 162 and regular. Lung sounds clear bilateral,Glucose 108, Bp 138/76, sp02 94%.
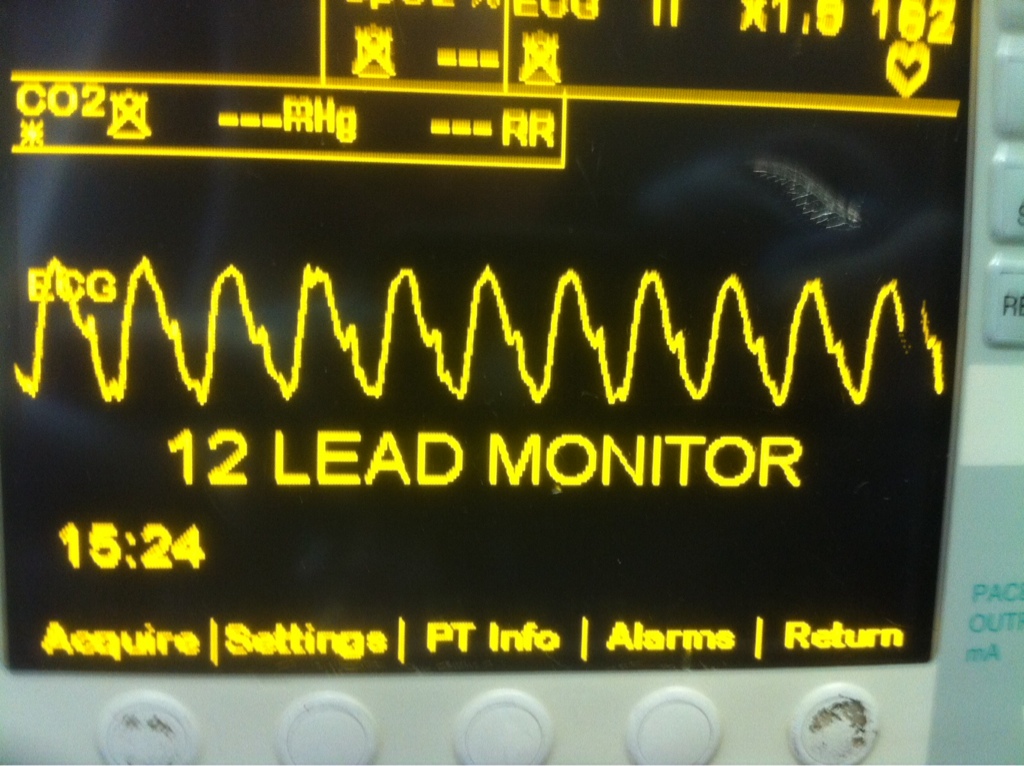
Initial 3 lead is this:
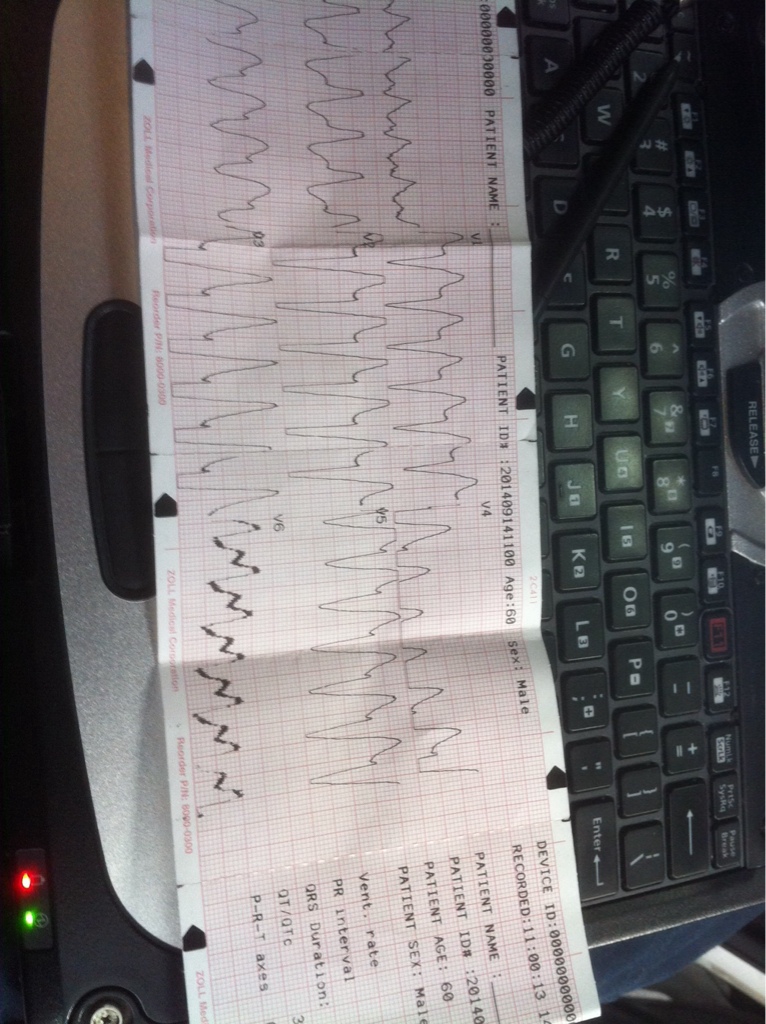
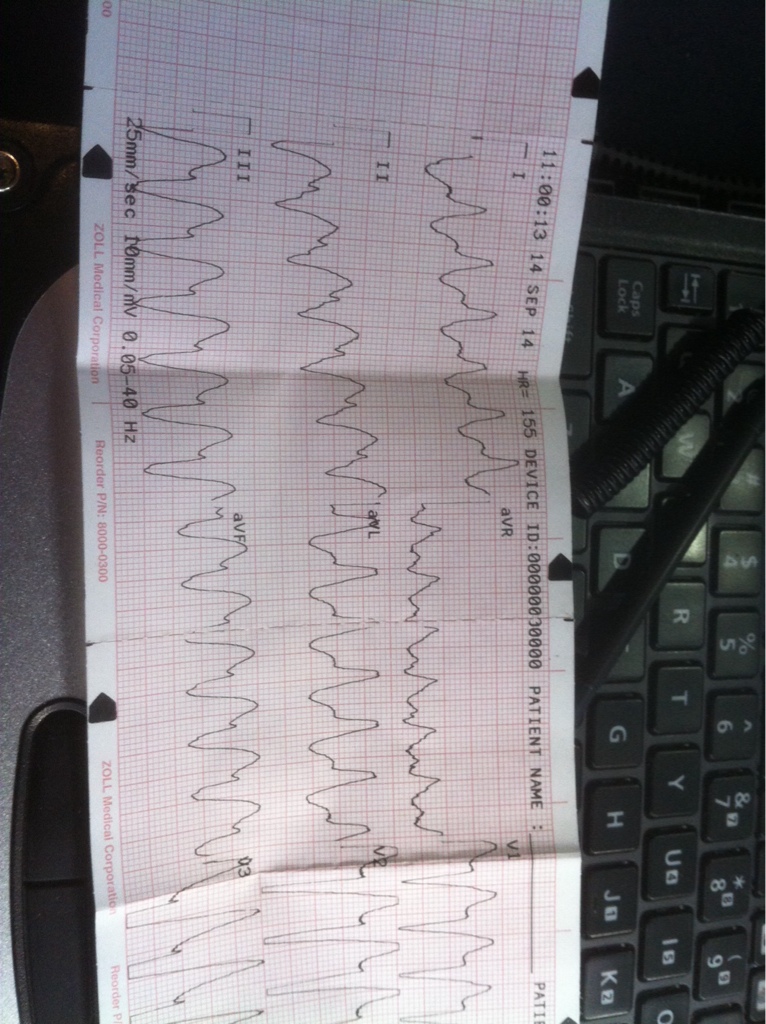
12 lead shows this:
You are 15 minutes from the hospital.
You start a line and administer 700cc of fluid with no change in rate.
How would you treat?
Upon arrival you find your patient sitting in her recliner in obvious distress. She states she feels very nauseated and sick to her stomach. Onset of this morning upon waking up. Hx of LBBB and implanted pace maker.
You palpate a pulse of 162 and regular. Lung sounds clear bilateral,Glucose 108, Bp 138/76, sp02 94%.
Initial 3 lead is this:
12 lead shows this:
You are 15 minutes from the hospital.
You start a line and administer 700cc of fluid with no change in rate.
How would you treat?
