Sorry for the confusion, LTAC stands for Long Term Acute Care, a facility that can provide acute and intensive care for >90 days. It's sort of a mix between a hospital and a nursing home, but considered a hospital by the government.
The patient is admitted for care of stage IV decubitus on her sacrum and legs. She also has a history of diabetes, hypertension and ESRD which she receives hemodialysis for.The patient takes atenolol,and is on an insulin sliding scale. An hour after receiving dialysis she was witnessed slumping over and found to be in cardiac arrest. The patient received CPR and one round of epi for PEA before regaining a pulse, the systolic B/P was found to be in the 60s so the patient was started on dopamine which was titrated "quickly" to 20mcg/kg/min, in addition the patient had received in the neighborhood of 3 liters of NS. The only access you have is a single lumen IJ where the dopamine is running. The patient was intubated with a 7.5 ETT placed to a depth of 22cm at the lips, vent settings are assist control at a rate of 24, vT of 400mls, PEEP of 5, FIO2 of 1.0 and a 1 second I time. The nurse tells you the patients doctor diagnosed a perforated bowel via chest x-ray. The patient is airborne isolation for MRSA, C.Diff, AND VRE (all the good stuff)
Physical exam shows a an unconscious intubated patient, GCS of 5 (E1, V1, M3).
Head is intact, an NG tube is in place draining draining dark green (and has appx 3l of drainage today). No JVD is present, in fact the jugular veins can't be palpated on the 55kg patient.
Breath sounds are equal, rhonchi is present in the right base, otherwise clear. No spontaneous respiratory effort seems to be present
Abdomen is non-distended, a colostomy and large surgical scar are present. A foley cath is in place, the patient has no UO today.
Extremities are intact except for the frank, multiple decubitus present on the legs.
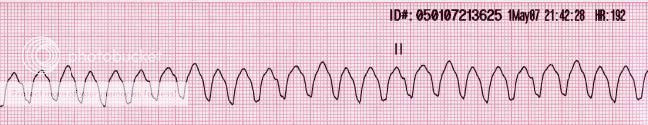
The current vitals are B/P 136/84 via NIBP, HR of 146, SpO2 of 100% and ETCO2 of 22 with a square waveform. No meds besides the epi or dopamine have been administered.
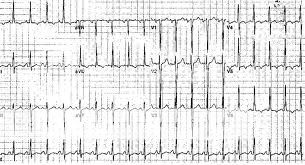
EKG:
No DNR, the family at beside is just saying "keep her alive, please". Transport time is 30 minutes, your partner is a medic but he has to drive, and is a graduate of a 10 week program and his only other EMS experience is as a non-transporting paramedic on a garbage truck

.