For EMS standards in my area, it's typically a max dose of 4 shocks with a manual defibrillator. 3 on the floor, 1 out the door as they say. However, certain circumstances are outlined when that may change.
1) Situations when you initiate rapid transport following 1 analysis:
- Arrest secondary to FBAO that cannot be cleared
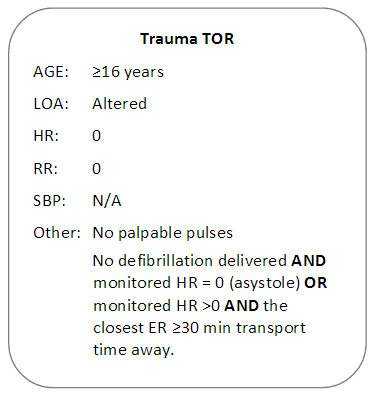
- Trauma cardiac arrest
2) Situations when you initiate rapid transport following the first non-shockable rhythm:
- Toxicological overdose
- Pediatric patients
- Anaphylaxis
The document has "etc" under the second category. I'd like to ask the community if you can think of any other situations you would initiate transport for a VSA patient after the first non-shockable rhythm you encounter.
1) Situations when you initiate rapid transport following 1 analysis:
- Arrest secondary to FBAO that cannot be cleared
- Trauma cardiac arrest
2) Situations when you initiate rapid transport following the first non-shockable rhythm:
- Toxicological overdose
- Pediatric patients
- Anaphylaxis
The document has "etc" under the second category. I'd like to ask the community if you can think of any other situations you would initiate transport for a VSA patient after the first non-shockable rhythm you encounter.