Any reason, other than what I mentioned, for not carrying just rocuronium? From the research I can find, the onset is about the same. Some say the intubating conditions are better with sux, but some say not... I think the data there is pretty subjective.
I couldn't say with any authority. Sux is whats used in EDs all over the country. It may just be that its the status quo and they extended it to MICA when RSI came in.
Ceftriaxone is a great choice to add! Totally forgot about this, but it is becoming a bigger thing, at least in CCT. Ceft is a great start, but also may also want quinolones, macrolides, and/or aminoglycosides for broad spectrum coverage since many of our patients are from nursing homes and have complicated infections of multiple or unknown source/system.
Any thoughts on carrying multiple antibiotics and administering for sepsis from an unknown organism?
Are you drawing cultures before administration??
I would suggest a respiratory quinolone like levofloxacin seeing as though community acquired pneumonia (CAP) constitutes the majority of sepsis case seen in the prehospital environment. But to be honest I don't know a great deal about this. Its my understanding that the particular drug used would be tailored to the local florae.
Perhaps also doxycylcine given its potential in both resp and urinary tract infections (septic nursing home patients with CAP or UTIs would constitute the bulk of sepsis case I would think).
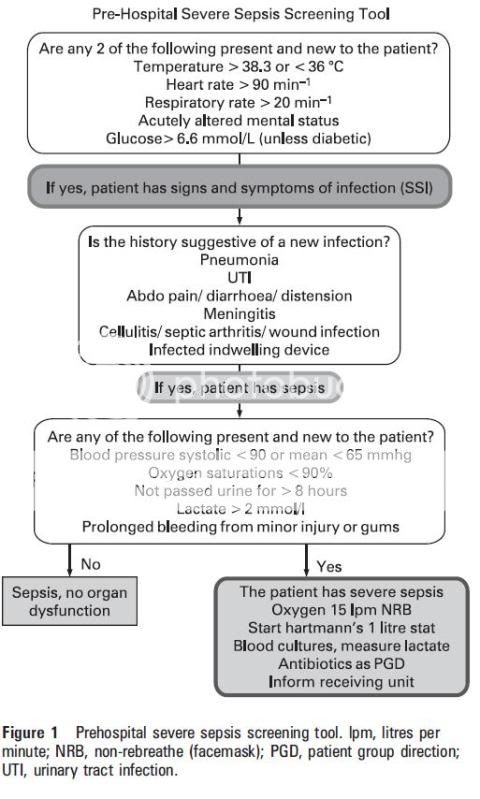
Although, I'm not sure of the necessity of utility of carrying such drugs on the average 000 truck. What I am more interested in is the idea of starting the management of the 'sepsis six' in the prehospital environment, in the hopes of expediting the process of the first 6 hours of evaluation and resuscitation, which in turn will expedite their ICU care should they need it.
1) ~100% O2 (currently we actually don't carry NRBMs, which I would like changed, personally).
2) Blood cultures (we don't currently draw blood cultures. I believe we should for two reasons. Firstly, it expedites a diagnosis if we can roll in the ED door with a bag ready to run off to the lab even while we're still waiting for a bed. Secondly, a blood culture taken before the ceftriaxone prevents the ED from encountering problems identifying the type of infection from sterile blood samples taken soon after the initial cef).
3) IV antibiotics (we have cef, for now I feel this is adequate, but the culture of not using it in the ambulance service needs to be addressed, Ambulance paramedics here, still do not appear to understand the way sepsis can creep up on you).
4)Fluid resuscitate (MICA can fluid resus a septic patient, basics cannot, although, you could easily argue dyhydration, or just plain step outside the guidelines - as long as you can back it up then that's fine. 2-3 rounds of 20mls/kg of a crystaloid appears to be the go in sepsis, and basics here are experienced in this modality for other conditions).
5)Serum Lactate and haemoglobbin. (obviously difficult in the prehospital environment. Although, there are relatively cheap, reliable portable lactate measuring tools apparently, and the suggest algorithm for sepsis triage (bellow) requires a lactate level).
6)Urinary cath + urin output (perhaps in rural mega transport time areas but otherwise I'd say this one can be left out [thoughts?], given that its a sterile and sometimes time consuming procedure).