- 7,886
- 2,858
- 113
You're dispatched to a residence for a 60 something male with shortness of breath. The patient's wife brings you to a basement living room where you find the patient seated in a recliner, alert, oriented, and mentating appropriately. Patient is on home oxygen at 2lpm. Wife tells you that the patient was recently diagnosed with pulmonary hypertension and has also been struggling with managing his CHF. The patient was admitted last week for pedal edema and ascites, patient was tapped and six liters taken off his abdomen. The patient informs you he is always mildly dyspneic but two hours ago he suddenly became more dyspneic and developed moderate chest tightness while watching TV. You work the patient up and note the following:
No other medical history. His medications include Lasix/KCL, sildenafil, and bactrim. Social history for alcoholism, patient no longer drinks.
Physical exam:
Skin: Pale, warm, dry. Jaundice noted.
HEENT: Atraumatic, pupils equal/round/reactive @4mm, jaundiced sclera.
Chest: Equal rise and fall. Pt appears cachectic. Basilar rales on left, otherwise clear throughout. No cough noted.
Abdomen: Significant distension with ascites.
Pelvis and back without remark.
Extremities: Upper without remark, strong and fast radial pulse. 4+ bilateral pedal edema with skin rupture and weeping. No way you can ascertain a pulse.
Neuro: Not remarkable.
Vitals:
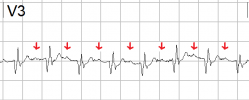
HR 184, BP difficult to obtain but eventually found to be 80/50 manually. 86% on 2lpm. Minor tachypnea noted. EKG attached.
What's next? What else would you like to know?
No other medical history. His medications include Lasix/KCL, sildenafil, and bactrim. Social history for alcoholism, patient no longer drinks.
Physical exam:
Skin: Pale, warm, dry. Jaundice noted.
HEENT: Atraumatic, pupils equal/round/reactive @4mm, jaundiced sclera.
Chest: Equal rise and fall. Pt appears cachectic. Basilar rales on left, otherwise clear throughout. No cough noted.
Abdomen: Significant distension with ascites.
Pelvis and back without remark.
Extremities: Upper without remark, strong and fast radial pulse. 4+ bilateral pedal edema with skin rupture and weeping. No way you can ascertain a pulse.
Neuro: Not remarkable.
Vitals:
HR 184, BP difficult to obtain but eventually found to be 80/50 manually. 86% on 2lpm. Minor tachypnea noted. EKG attached.
What's next? What else would you like to know?