- 2,735
- 1,272
- 113
I'm happy to give a scenario and/or more background information later, but I initially want to see what everyone thinks of these recently acquired EKGs.
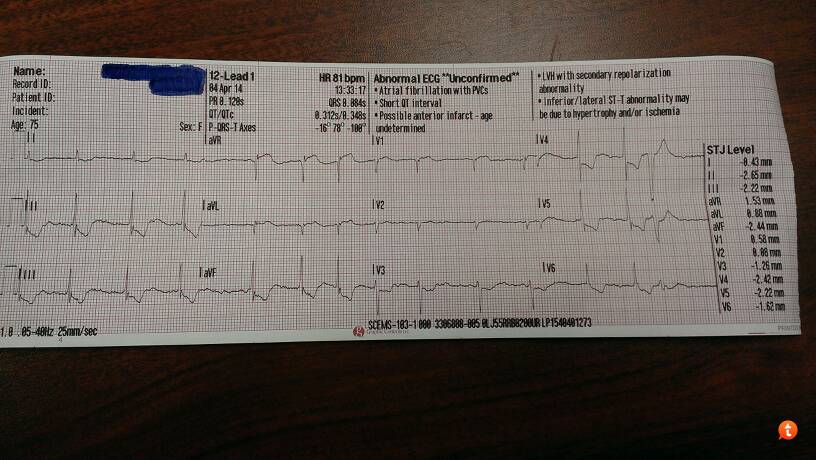
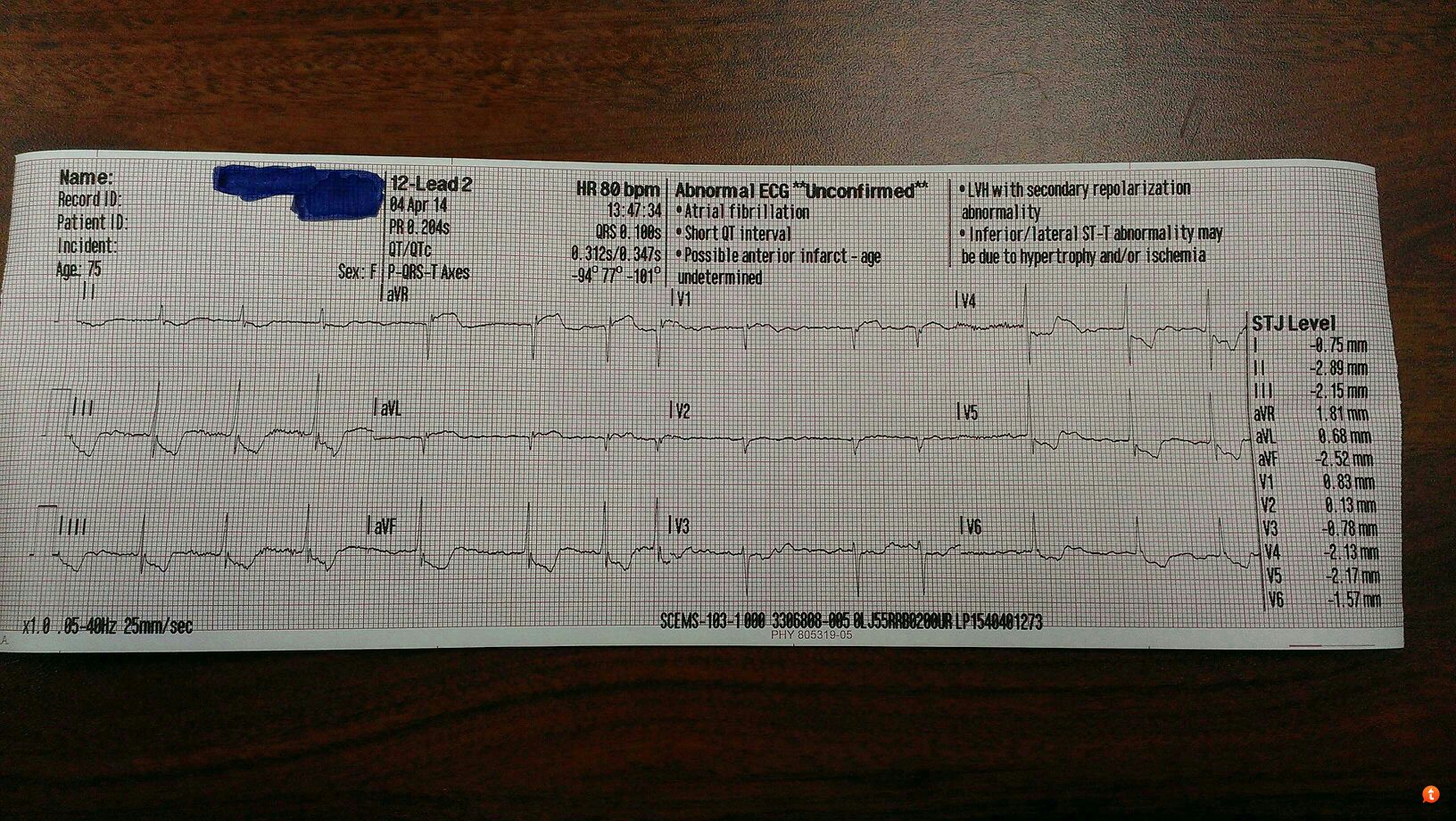
Anyone have any thoughts?
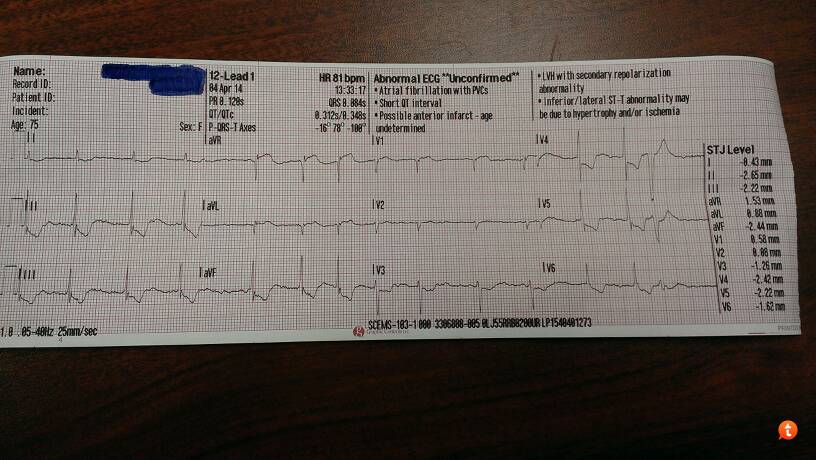
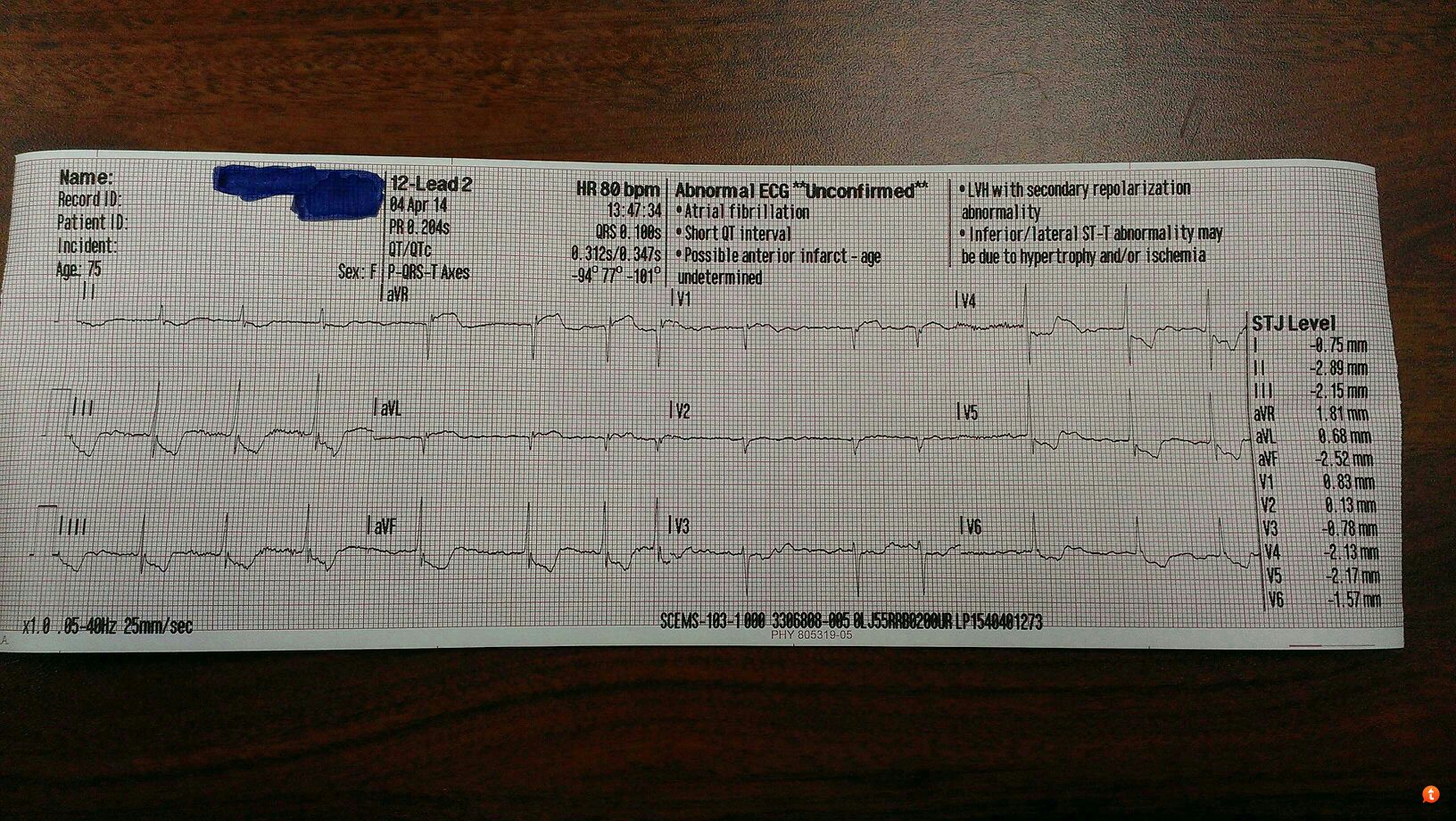
Anyone have any thoughts?

