- 2,735
- 1,272
- 113
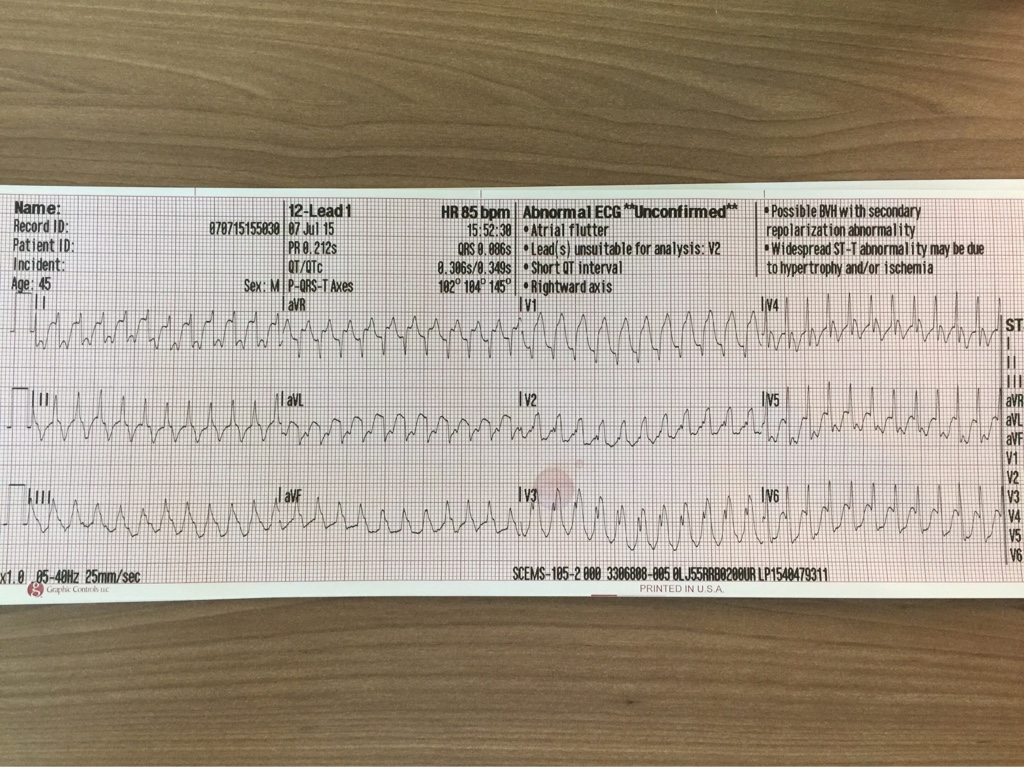
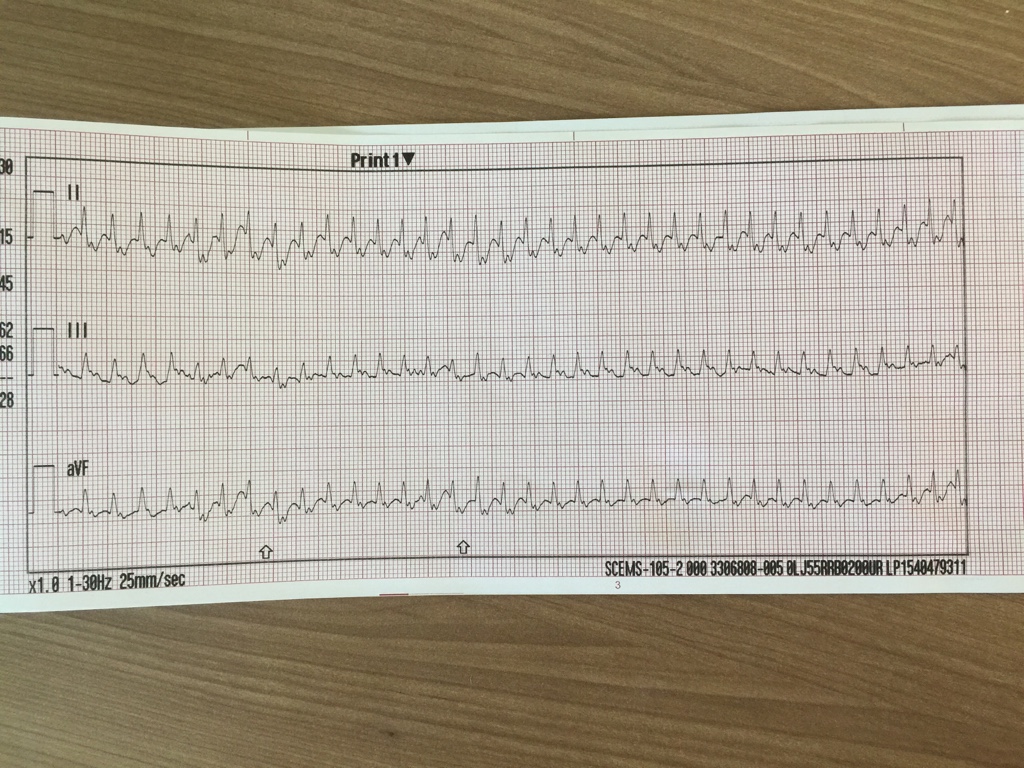
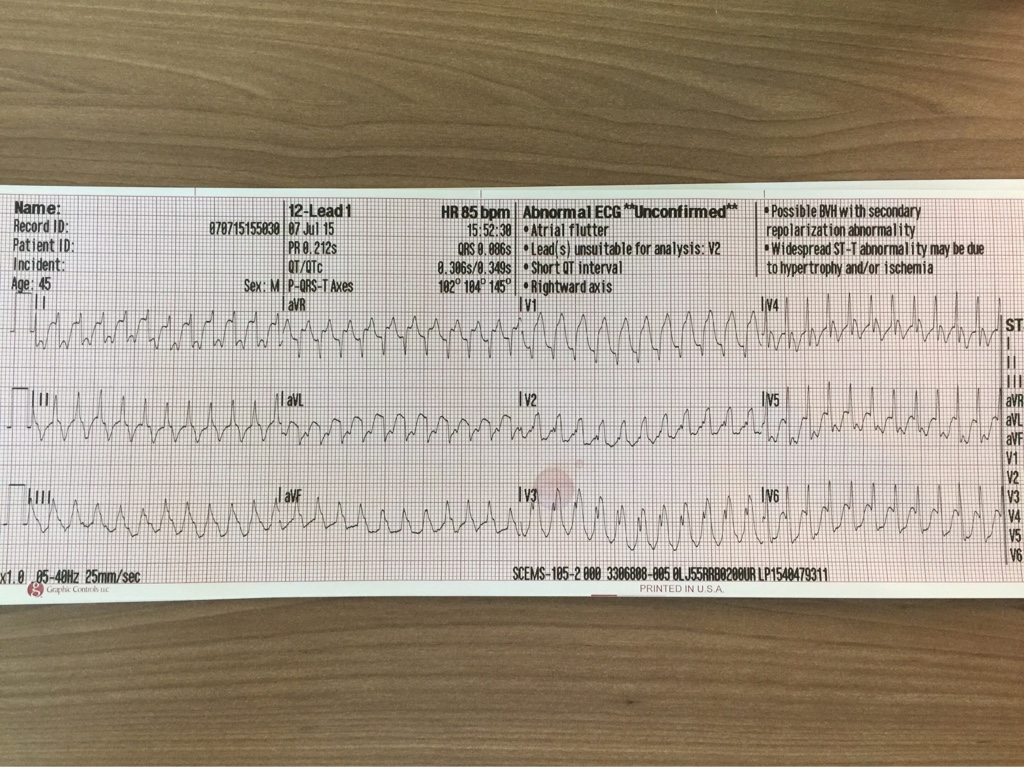
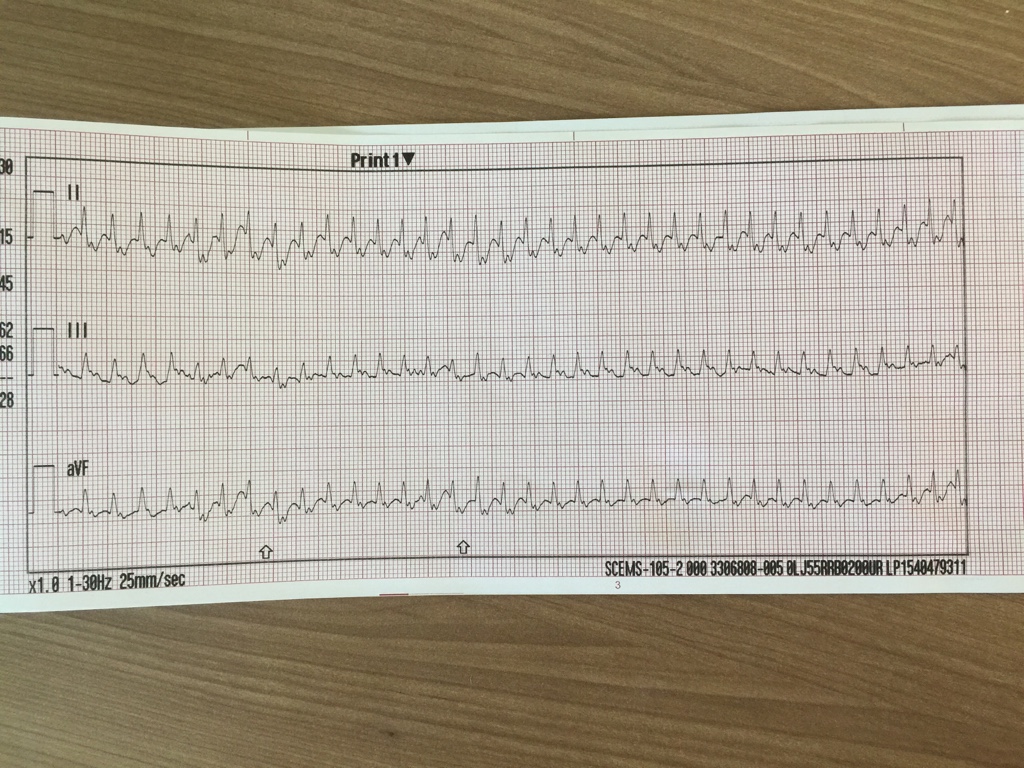
Here's one for the EKG buffs. This is an absolutely cold read, as my partner and I literally found this EKG in the trash can at our station this AM. We know it's a 45 year old male as that information was input to the monitor, but we have no clinical scenario, symptoms, history, or vitals of any kind. My partner and I interpreted this rhythm differently, so I'd love to see a little discussion about it on here. Without further ado, here's the single 12 lead we have and a rhythm strip.