- 9,736
- 1,174
- 113
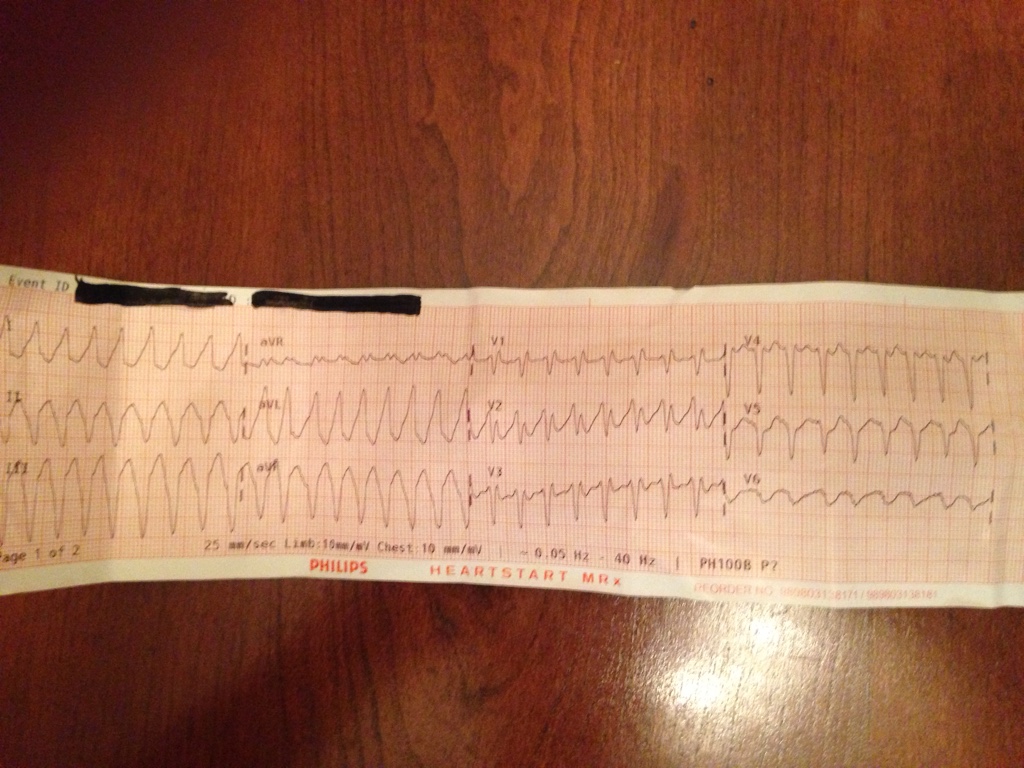
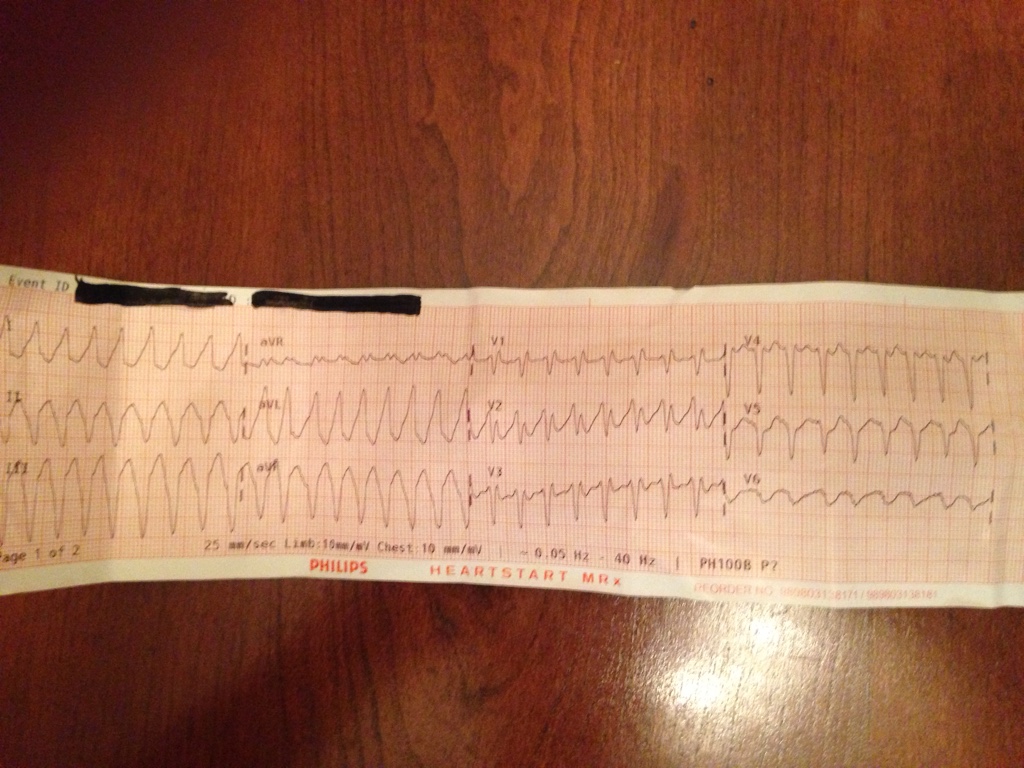
58 year old male presents with non-radiating/reproducible retrosternal chest pressure ranging from a 4/10 to 8/10 with associated SOB and diaphoresis. Started 30 minutes after a 'normal' hour long workout. Reduced with rest then increased 15 minutes after taking the trash down a flight of stairs to the dumpster and returning to his apartment which happened 5 initial onset. PT has had similar episodes over the last 3 months with 'normal' echocardiogram and stress test within the last 4 weeks.
PT is GCS 15 cool, pale and diaphoretic. Physical exam is otherwise unremarkable.
Vitals:
112/90
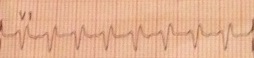
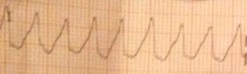
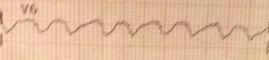
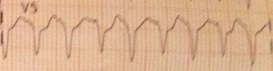
HR as seen at 210 with corresponding pulses.
96% on room air
RR 34 with clear lung sounds bilaterally.
History:
HTN
MI "a few years ago" with stent x2 in RCA
Chronic back pain
NKDA
Meds:
Lisinopril
Flexeril
Hydrocodone/APAP
Non-smoker, rare social ETOH, no drug use
PT is GCS 15 cool, pale and diaphoretic. Physical exam is otherwise unremarkable.
Vitals:
112/90
HR as seen at 210 with corresponding pulses.
96% on room air
RR 34 with clear lung sounds bilaterally.
History:
HTN
MI "a few years ago" with stent x2 in RCA
Chronic back pain
NKDA
Meds:
Lisinopril
Flexeril
Hydrocodone/APAP
Non-smoker, rare social ETOH, no drug use