LocNar
Forum Probie
- 15
- 2
- 3
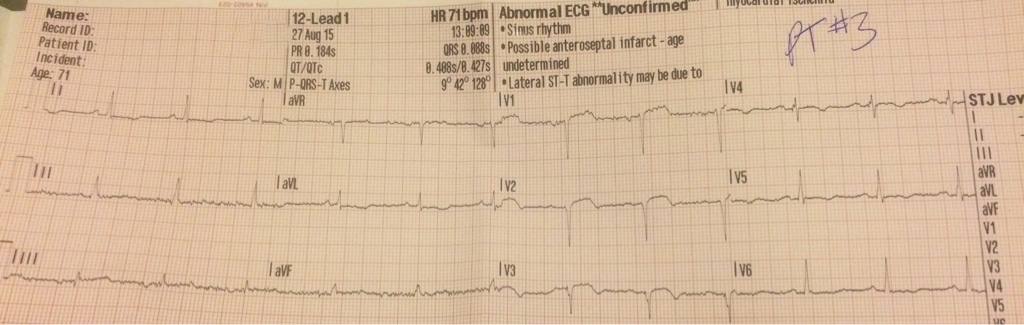
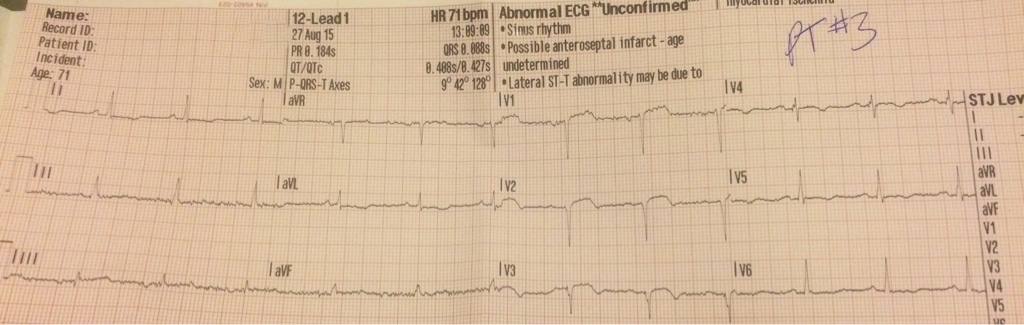
71yoM gets out of his car, stands up passes out, hits the concrete. Patient wakes up after hitting the ground, complains of left shoulder pain and states he can't move it. Some minor abrasions are present on the arm, patient denies any head, neck, or back pain. Patient has a past history of two silent MI's, and two stents. Stage 4 colon cancer in the past with a removal of four feet of guts. Sit the patient up to stand him up, color drains from his face, and he vomits. Lay him back down color returns patient feels fine. Transfer him to the back of the truck, BP: 110's systolic while flat, HR: 76, O2 says 96% on RA. 4 lead shows sinus rhythm. Sit the patient up to sling and swathe the left arm, color drops patient vomits again, pressure drops to 80's systolic. Lay him back down, color returns, patient feels fine. Pressure comes back up to low 100's systolic. Lung sounds clear all over, IV started, bag o'fluids hung. Pressure stays in the 110's. 12 lead shows small amount of elevation in Two leads. It was noted and passed along to the receiving facility. Would you feel comfortable treating this as a STEMI?